Office Procedures
There are many procedures, including minimally invasive procedures that can be done safely and conveniently in the office. These include procedures for the evaluation and treatment of an abnormal pap smear and irregular or excessive vaginal bleeding. Minimally invasive permanent sterilization is also done in the office. Below are links for comprehensive information on each procedure.
In office procedures:
- Treatment of heavy bleeding (Novasure®)
- Colposcopy for the evaluation of abnormal pap smears
- LEEP
- IUD insertion (Mirena®, Skyla®, Paragard®)
- Endometrial biopsy
- Ultrasonography
- Sonohysterograms
- Laboratory Services
Endometrial Ablation
What is endometrial ablation?
Endometrial ablation is used to treat heavy bleeding. It destroys a thin layer of the lining of the uterus (endometrium) and stops or reduces the menstrual flow in many women. Heavy bleeding is often treated first with hormones, such as birth control pills. Endometrial ablation is a non-hormonal treatment option for women who cannot tolerate or do not desire hormones.
The procedure can be done as an outpatient at the hospital or in our office with sedation. Virtually no recovery is needed. A number of different techniques are available and the Women’s Group of Northwestern offers the Novasure and Thermachoice as safe options.
What to do to prepare for endometrial ablation?
Your doctor will help determine if endometrial ablation is the right treatment option for you. When you have your consultation for heavy bleeding, the provider will require an ultrasound. This is done to evaluate the size and shape of the uterus, but also rule out any other causes of bleeding, such as uterine fibroids or endometrial polyps. An endometrial biopsy is also required to ensure there are no pre-cancerous or cancerous cells present before scheduling an ablation.
The day of the procedure you will receive sedation so you may not eat or drink anything for 6 hours prior. Someone must accompany you to the office and be available to take you home.
Who should not have endometrial ablation?
Endometrial ablation is not recommended for women with the following medical conditions:
- Disorders of the uterus or endometrium
- Endometrial hyperplasia
- Cancer of the uterus
- Recent pregnancy
- Current or recent infection of the uterus
- Women who desire their fertility – pregnancy is not likely or recommended after ablation, but it can happen
- Postmenopausal women
What to expect after the procedure?
Cramping, like menstrual cramps, for 1-2 days are not uncommon. Also, thin, watery discharge mixed with blood can last a few weeks. If you experience heavy bleeding, fever, severe pain, persistent nausea or vomiting or abdominal distention, call the office.
Novasure
This a simple and safe device that is used to destroy the uterine lining, which puts an end to heavy, uncomfortable menstrual bleeding. Patients experience a quick recovery as no incisions are made and there is no need for general anesthesia. Following the procedure, many women no longer have menstrual cycles.
GYNECARE THERMACHOICE® Uterine Balloon Therapy System
One effective treatment for heavy periods is a global endometrial ablation (GEA) procedure called GYNECARE THERMACHOICE® Uterine Balloon Therapy System. GYNECARE THERMACHOICE® is an effective, nonhormonal, permanent treatment for heavy periods. It involves a minimally invasive, 8-minute procedure that can be performed in your doctor’s office or in a hospital.
Studies have shown that:
- 81% of women treated with GYNECARE THERMACHOICE® returned to normal levels of menstrual bleeding or lower
- 89% of patients had a reduction of menstrual pain and cramping
- 96% of patients reported satisfaction with GYNECARE THERMACHOICE® III
GYNECARE THERMACHOICE® is a soft, flexible balloon that a doctor inserts in the uterus (womb) to treat the endometrium, the lining of the uterus. GYNECARE THERMACHOICE® is an effective, nonhormonal treatment for heavy periods. It involves a minimally invasive, 8-minute procedure that can be performed in your doctor’s office or in a hospital. There are a number of options for managing heavy periods. Most doctors recommend birth control pills or an IUD initially to manage heavy periods, but for many women, these options are either ineffective or undesirable. They can cause weight gain, moodiness and breast tenderness, and may not ultimately be effective in reducing heavy periods.
Colposcopy
Colposcopy is a special examination of the cervix performed when there is an abnormal pap smear. The cervix is prepared with special stains to make abnormal cells stand out. Sometimes a biopsy is performed to evaluate those cells further. This exam is performed right in the office.
What to Expect: A speculum is inserted like with a Pap smear and the cervix is visualized directly through the colposcope. You may experience a pinching sensation and/or cramping as samples are taken from the cervix.
Preprocedure: (before) Eat regular meals. You may take over-the-counter pain medication 60 minutes prior to the procedure.
Post procedure: (after) You may have mild cramping. Expect light bleeding and a yellow, mustard-like or coffee ground-like vaginal discharge. This is due to a solution put on the cervix to stop bleeding. We will advise you not to put anything in the vagina or exercise for 2-3 days. Biopsy results are usually available 7-10 days after the procedure.
Colpo – Printable Instructions, click here
LEEP
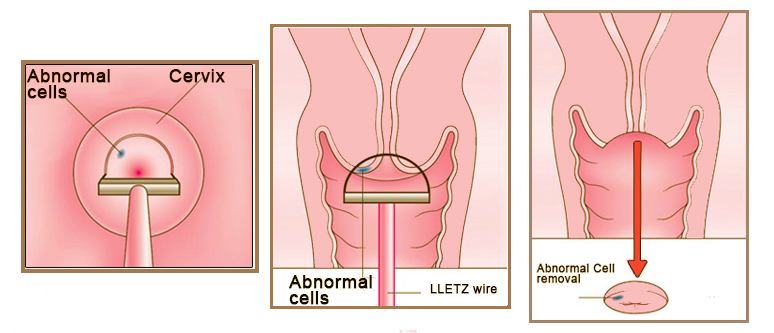
LEEP is also known as Loop Electrical Excision Procedure. LEEP is one type of procedures used to diagnoses and treatment abnormal cervical cells. This procedure is used most often for treating moderate to severe dysplasia (abnormal changes of the cells lining the cervix or precancers) that have been identified by colposcopy and/or cervical biopsy.
What to Expect: (before)
The cervix will be numbed with medication and abnormal cells removed. Mild cramping
may occur.
Preprocedure:
Eat regular meals. You may take over-the-counter pain medication 60 minutes prior to
the procedure.
Post procedure: (after)
You may have mild cramping. Expect light bleeding and a yellow, mustard-like or coffee ground-like vaginal discharge. This is due to a solution put on the cervix to stop bleeding. A small amount of tissue may pass as the cervix heals. We will advise you not to put anything in the vagina or exercise for 2 weeks. Biopsy results are usually available 7-10 days after the procedure.
Leep – Printable Instructions, click here
IUD insertion
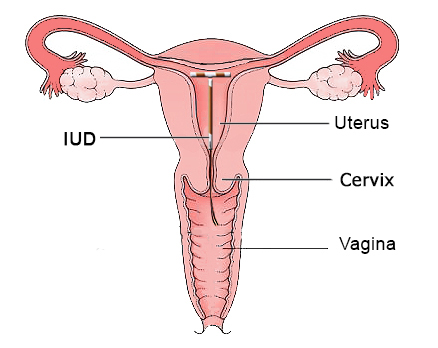
The IUD prevents pregnancy by interfering with the movement of the sperm inside the uterus and the progestin prevents some women from ovulating (releasing an egg) at all, thus preventing the possibility of pregnancy. The IUD is a good option for women who want to avoid hormonal systemic methods of birth control, do not desire a pregnancy for an extended period of time and want the convenience of not having to do anything on an ongoing basis.
What to expect: A speculum will be place in the vagina as with a Pap smear. The cervix will be cleansed with an antiseptic solution before the device is inserted. Cramps, dizziness, and/or some bleeding may occur and are common side effects
Preprocedure: (before) Eat your regular meals. You will be advised to take ibuprofen, Aleve or Motrin 2-3 hours prior to the procedure. Ask the provider at your consultation if additional medications are recommended.
Postprocedure: (after) Some cramping and bleeding can be expected. Ibuprofen can be taken every 6 hours to help with any discomfort.
IUD – Printable Instructions, click here
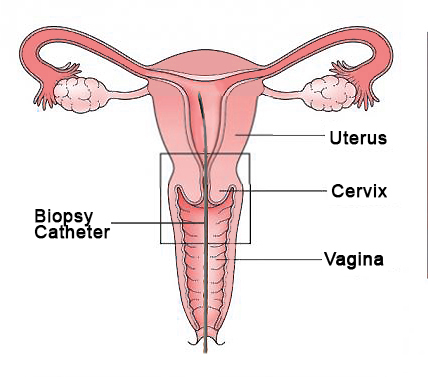
Endometrial Biopsy
The endometrial biopsy is an office procedure that is used to remove a sample of the lining of the uterus. The tissue subsequently undergoes a histological evaluation at the Northwestern Memorial Hospital pathology department which is supplied to the physician to aid in the diagnosis. Endometrial biopsy is usually done to investigate abnormal uterine bleeding. Your physician will take tissue samples from the inside of the uterus using a thin hollow catheter. The procedure can cause cramping for about five minutes and subsides quickly.
What To Expect: A speculum will be place in the vagina as with a Pap smear. The cervix will be cleansed with an antiseptic solution before the device is inserted. We pass a thin catheter that goes through the cervix into the uterus to get a sample of tissue. It may cause discomfort for about one minute.
Preprocedure: (before) Eat your regular meals. You may take a pain medicine 30-60 minute prior to the procedure. This could include over-the-counter Aleve, Advil, or Motrin.
Postprocedure: (after) You may have mild cramping. Expect vaginal discharge. We will advise you not put anything in the vagina or exercise for several days. Biopsy results are usually available 7-10 days after the procedure.Endometrial biopsy – Printable Instructions, click here
Sonohysterograms
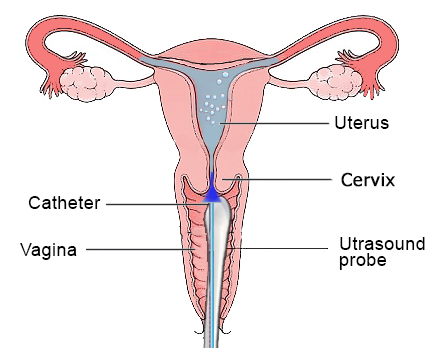
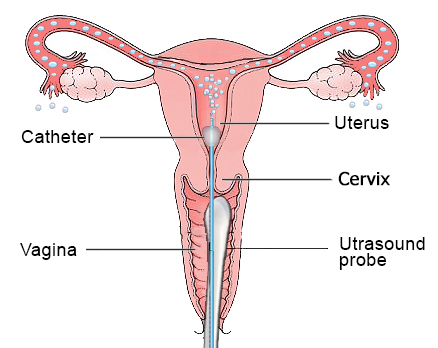
A Sonohysterogram consists of imaging of the uterus and uterine cavity using ultrasonography while sterile saline is instilled into the uterine cavity. A small plastic catheter (a hollow tube) is connected to the container of saline solution and then inserted through the vagina into the uterus. The saline is introduced into the uterus to distend the cavity to allow careful examination of the uterine structures and lining while using the transvaginal ultrasound probe.
Why a Sonohysterogram: Many times a Sonohysterogram is scheduled after a standard ultrasound, a trans-vaginal ultrasound or an endometrial biopsy have already been performed. A Sonohysterogram can help diagnose many medical issues including uterine polyps, fibroids and blocked tubes. You will need to plan your appointment around your menstrual cycle. Your Sonohysterogram appointment should be scheduled for the fifth through the eleventh day of your menstrual cycle.
What to expect: A speculum will be place in the vagina as with a Pap smear. The cervix will be cleansed with an antiseptic solution before the device is inserted. Cramps, dizziness, and/or some bleeding may occur and are common side effects
Preprocedure: (before) An hour before your appointment you will want to take a pain relieving medication such as ibuprofen or acetaminophen. Pre-medicating will help reduce the amount of pain from cramping during the Sonohysterogram.
Postprocedure: (after) After your appointment you may experience mild to moderate saline discharge, cramping and spotting. Having a pad ready to use after the procedure will make you feel more comfortable.
Sonohysterogram – Printable Instructions, click here
FemVue Sono HSG
FemVue, also known as a sono-hysterosalpingogram, is done under ultrasound in the office to evaluate the uterine cavity and Fallopian tubes for women undergoing a fertility evaluation and is being done in place of the HSG for some patients. Unlike the HSG, FemVue does not require X-ray and is done in the office, eliminating a trip to the hospital. The procedure is performed during the first half of your menstrual cycle, after menses has ended but before ovulation, usually between cycle days 6 and 11.
What to Expect: First we do a traditional vaginal ultrasound to measure the uterus, look at the muscles of the uterus, measure the ovaries and make sure the ovaries appear normal. Then a speculum is placed in the vagina, the cervix is cleaned and a thin plastic catheter is placed through the cervix into the uterus. Then while watching with ultrasound, a small amount of saline is injected into the uterine cavity so we can see the uterine anatomy and see if there’s anything inside of the uterus that could prevent the pregnancy from occurring. We can also instill some bubbles into the uterine cavity and see if the bubbles pass through the Fallopian tubes so we can evaluate if the Fallopian tubes are open.
Preprocedure: (before) The procedure takes approximately 15-20 minutes. We recommend ibuprofen or Aleve 30 minutes prior to procedure with some food.
Postprocedure: (after) You may experience menstrual like cramps, spotting and drainage of saline after the procedure.
FemVue Sono HSG– Printable Instructions, click here
Vulvar Biopsy
A vulvar/vaginal biopsy takes one or more samples of tissue from the vulva. The vulva is the outer parts of the female genitals, including the labia, which are often called the lips, and the clitoris. The vagina is the opening that leads to the cervix, which is the entrance to the uterus. A biopsy is done to determine why you may have noticed itching, redness, swelling or changes in color to your vulva or vagina. It may also be done if you have a lump or sore that has recently appeared.
What to expect: The biopsy area will be cleaned with an antiseptic liquid. If you are having a vaginal biopsy, your provider will use a speculum to open your vagina. A speculum is the same instrument used during a Pap smear. Numbing medicine will be injected into the area that is going to be biopsied. One or more small pieces of tissue will be removed and sent to a lab for analysis. If you require stitches, dissolvable stitches will most likely be used, which do not need to be removed by your provider. You may feel some discomfort and pressure during the procedure.
Preprocedure: (before) Unless otherwise instructed, you do not need to do anything special before the biopsy. However, if you have the chance, it would be good to have a bath or shower on the day of the biopsy and to wash the skin gently but thoroughly. It will help to wear comfortable clothes and bring a panty liner.
Postprocedure: (after) Keep the area as clean and dry as possible. You may bathe or shower the next day. Gently pat the area dry with a clean towel.